Our Approach to post COVID-19 Syndrome: a clinical perspective
We have been working with post-Covid-19 Syndrome (PC19S) from the moment we realised persistent fatigue was an issue in Covid-19. Since then, as well as having our own caseload of long Covid patients, we have developed a partnership with the University of East Anglia (UEA) and created a research study, contributed to national guidance, led training programmes, have offered supervision for healthcare professionals, and are delivering early intervention programmes and return to work programmes.
How our programmes support people with post-Covid syndrome
Until research informs us, we don’t yet have an evidence base for how to manage post-Covid syndrome. We use our experience in managing other post-viral illnesses. We use our clinical judgement regarding this novel illness and we continue to reflect and adapt our approach. We collect data, outcomes, and share the practice with peers.
We draw on positive and credible information sources such as those from the NHS, Royal College of Occupational Therapists, British Medical Journal, National Institute for Health and Care Excellence (NICE), gov.uk, and the British Association for Chronic Fatigue Syndrome/ME (BACME) amongst others.
What do guidelines worldwide agree are the best management strategies for post-Covid syndrome?
Guidelines worldwide agree on a number of strategies, mostly:
Specific Covid-appropriate assessment
Fatigue management, including pacing
Rest and relaxation in the acute phase
Gradual reintroduction of activities
Managing breathlessness
Managing anxiety
Setting a daily routine
Exercise (with some caveats)
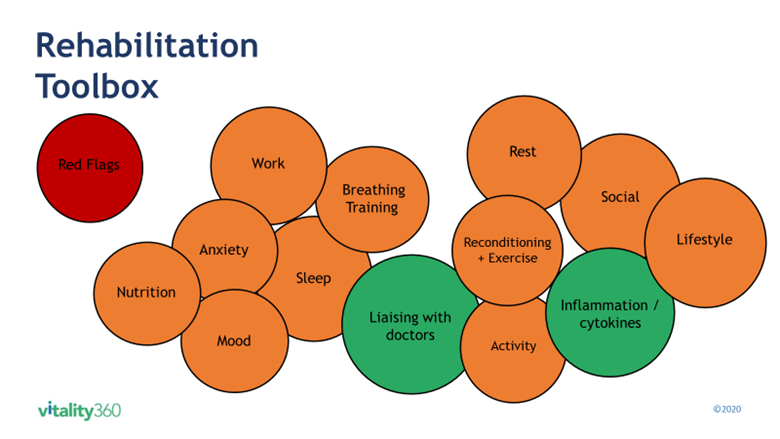
Clinical judgement in our rehab programmes
Dealing with how the individual patient presents at the time and drawing on our experience in assessment includes their medical history combined with psychosocial factors such as work, sleep, anxiety etc. We focus on the whole person and the complete picture and our programmes are collaborative and bespoke according to each individual’s needs and aspirations.
We assess for specific current stressors and support people in discussing, managing, and problem-solving where needed. This could include:
Offering hope
Vocational implications including managing a graded return to work
Support for parents eg around home-schooling
Financial discussions
Ergonomics
Sleep
Managing red flags
We assess and manage red flags, medical and psychological, by looking for new, deteriorating or persistent cardiac, respiratory or neurological signs. We act on anything that appears clinically concerning, including weight loss, and help people understand when they might need to escalate to increased medical assessment. We assess for any risks associated with higher levels of aerobic exercise and encourage people to start slow, go slow and stop and check if they experience concerning symptoms. It’s important that we remain flexible and adjust our approach according to new or emerging data.
A collaborative approach is crucial
Post-Covid syndrome affects a range of body systems and can also have a profound impact on emotional wellbeing. Working in collaboration with other healthcare professionals, such as medical consultants (eg respiratory, neurological, cardiac, ENT) is therefore essential. This may also include psychologists and other related practitioners, vocational consultants, employers and speech therapists.
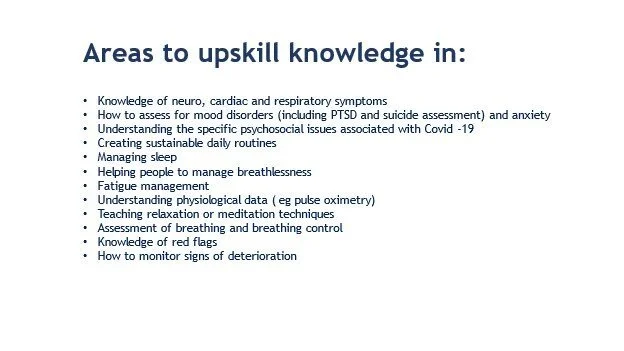
What do we need to keep learning as more is known about this condition?
How we are adding to the evidence base
We are contributing to the global evidence base by designing a study (Vitality360 partnership with UEA). We also run seminars on the management of long Covid and how to support a return to work for those with this condition, drawing on our expertise in this area, and we provide supervision opportunities for health professionals.
Our clients report great improvement at the end of our programmes. Read more in this Case Story here about Beth’s journey.
Written by Jessica Bavinton, Specialist Physiotherapist in Fatigue and Pain and Founder/Director of Vitality360