How to live with Cognitive Dysfunction/brain fog as part of long Covid
A high percentage of clients we are seeing with Long Covid describe cognitive dysfunction as one of the main symptoms they are continuing to experience. This is consistent with the recently published paper, ‘Characteristics of Long Covid’ by Nida Ziauddeen et al.
Characteristics of Long Covid’ by Nida Ziauddeen , Deepti Gurdasani , Margaret E O’Hara , Claire Hastie , Paul Roderick , Guiqing Yao , Nisreen A Alwan.
Typically, cognitive dysfunction includes difficulty with concentrating or sustaining attention, short term memory, word finding, complex cognitive thinking, problem solving, and losing the thread during conversations. We do not yet know if there are any biological reasons why cognitive functioning is affected by Covid 19. However, as Clinicians who have worked with clients with CFS/ME and fibromyalgia for many years the description of these symptoms, the words our clients use, the variability and the impact seem very familiar. Phrases that clients have used to describe cognitive dysfunction have included:
Treacle in my head
I don’t have ANY thoughts in my head, just a blank space
The little person in your brain who usually finds words and strings them together into sentences either a) runs around waving their arms about and still can’t find the right filing cabinet or b) just sits down and stops with their arms folded!
Like everyone is trying to communicate with me using smoke signals
My head feels heavy and as though it is floating just above me – all at the same time
These symptoms impact on all activities of daily living and make concentrating, carrying out tasks and communicating difficult. The following comments reflect our clients’ experiences of the way it impacts them:
I sometimes struggle to understand really simple instructions and sentences and struggle to be decisive, even simple choices like do I want a cup of tea
I feel as though I am staring blankly at the person who is talking to me
Reading one page can take several attempts
I make stupid mistakes – like pouring water from the kettle on to the kitchen worktop not in the cup!
I lose spatial awareness – like walking into door frames
I can find a word but I know it isn’t the right word
To paraphrase Morecombe and Wise – I know all the right words, but not necessarily in the right order!
One of the key things that they want to make us aware of is that this cognitive dysfunction can fluctuate, so there are also times that these symptoms are less problematic.
So how do we support clients to manage their cognitive fatigue and improve their functioning?
We encourage our clients to notice whether there are any triggers to their Long Covid symptoms including cognitive dysfunction. For many, there does seem to be a correlation between what they do and these symptoms. Too much cognitive effort without a break can result in increased symptoms – at times this is observable within a 1-hour Zoom appointment. It seems obvious and we can perhaps all relate to it, but clients also say physical exertion, or generally doing too much, can impact cognitive functioning.
Others describe feelings of anxiety or low mood as triggers. Building awareness of individual triggers can help to manage these symptoms.
In addition to being aware of triggers, we also advise clients to notice when their brain is functioning. When we are concerned about something we can become overly focused on this and spot all the times we get it wrong, even when at times no-one else will have noticed. We encourage people to also notice when they get it right - when they remember what they went to the fridge for; when they remembered how to drive the car; when they remembered how to cook dinner, for example. We also encourage people to notice the variance in their cognitive ability – at times the brain is still sharp.
Strategies to help
We talk to our clients about strategies to help minimise the amount of cognitive fatigue they experience. For example, to reduce complex cognitive tasks for a while and engage in activities that use the brain but are less demanding. This might be to read a magazine or short stories rather than a novel, watch a tv programme that is light rather than a heavy drama with a complex plot.
It is helpful to build up to more complex activities slowly and to split cognitive tasks into manageable chunks, e.g. work on a task for 30 minutes then take a break, stretch or move, and practise relaxation and/or grounding strategies to calm the mind.
Practical solutions can be both ‘high tech’ and ‘low tech’, for example:
Phone or computer apps (e.g. Evernote, Google Keep, Cozi, Colornote)
Using phone reminders
Writing reminders and to-do lists on sticky notes
Cognitive dysfunction and coping with a return to work
Clearly, the effects of cognitive dysfunction are particularly problematic when returning to work, or trying to remain at work. Many of our clients’ job roles include high levels of sustained cognitive effort throughout the working day. Some describe their cognitive functioning before Covid 19 as very sharp, quick, able to multi-task, with fast recall. The cognitive dysfunction is a barrier to them managing their normal occupations but many also say they are anxious about what employers/colleagues will think if they are not performing tasks up to their usual high standard.
Most of the tools and strategies used at home, like having breaks and setting reminders, are also beneficial to managing cognitive fatigue at work. Other suggestions that clients have found helpful include:
Recording meetings - if people give permission (explain what you want it for and what you will do with the recording when you have listened to it)
Follow-up conversations with an email (just to confirm our discussion, we agreed that x was happening at y time and I need to do z – is that what you understood too?)
If possible, if there are ‘better’ and ‘worse’ times of the day then arrange workload to take that into account
Stop for a cuppa or snack (healthy obviously!)
Mindmaps (either software or pen and paper) that help get thoughts into some order
Managing the environment (light, noise/noise-cancelling headphones) to minimise fatigue and help with concentration
Finding ways of creating space from interruptions. One client and her manager used a small toy on her desk – if it was on the desk don’t interrupt; if it was in her drawer, it was fine to interrupt (and she didn’t have brain fog!)
Communication with managers around work performance
Many clients express concern about how they think managers and colleagues will perceive their ability and competence because of the impact of their cognitive fatigue. People can be reluctant to put strategies in place because they feel that it will draw attention to them as being different. But when looking around most workplaces it becomes apparent that many people use tools to help them remember things, organise their workload, etc. whether that is a reminder on Outlook, mindmap software, to-do lists, or sticky notes. They won’t be the only ones!
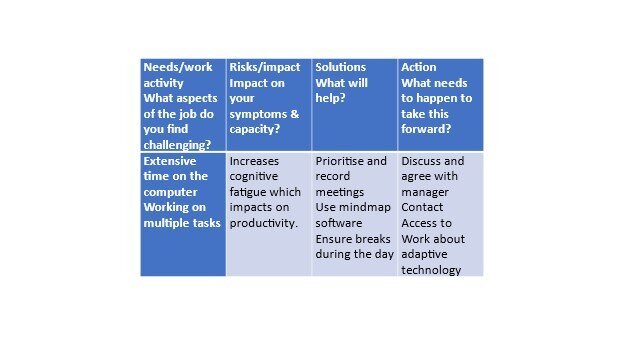
Challenges, needs, solutions framework for supporting work activities with cognitive dysfunction
A solution-focused approach to communication
Using a solution-focused approach to communicating about the impact of cognitive fatigue can help at work. We suggest using this framework when talking about the impact of symptoms:
It may not be necessary to communicate this amount of detail with everyone but it can be helpful to let people know if you are having particular difficulty concentrating on a task or conversation – “I’m sorry, I’m struggling to concentrate at the moment, can we have a quick break while I get a drink”.
‘Capability versus capacity’
Our Career and Employment specialist often uses the phrase “capability versus capacity” to remind and reassure clients that it isn’t that they have become stupid or any less capable, but their capacity has changed, and the way they undertake tasks has changed.
The good news is that many of the clients we are working with are already seeing a significant improvement in their memory, concentration, word-finding, and thinking. We believe this is not just due to time but also due to developing a greater understanding of these symptoms, identifying triggers and incorporating management strategies into daily living.